ITB Friction Syndrome is one of the most common overuse injuries affecting runners and cyclists. Despite its prevalence, this injury still gets very little exposure and is understood by few people outside sufferers and practitioners.
WHAT IS THE ITB?
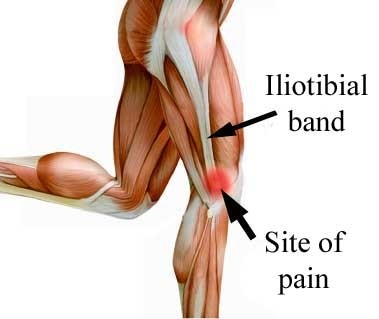
The iliotibial band (ITB) is a thick, fibrous band of connective tissue which spans from the outside of the pelvis, down past the knee to attach to the top, lateral aspect of the shin bone (tibia).
The ITB functions as an extension of and attachment site for the tensor fascia latae and gluteus maximus muscles; assisting in providing lateral stability to the knee when standing and, especially, through the stance phase of gait.

WHAT IS ITB FRICTION SYNDROME?
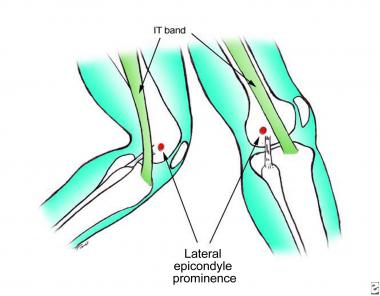
As is obvious from the name, ITB friction syndrome (ITBFS) involves a point of friction between the distal (knee) end of the ITB and the lateral epicondyle of the thigh bone (femur), a small bony protrusion arising from the outside aspect of the bone. It is this rubbing which causes the inflammation and pain indicative of ITBFS.
There are different schools of thought regarding the actual pathophysiology of the syndrome. The more common and long-standing theory is that inflammation of the ITB fascia occurs and this is what causes the symptoms.
However, a new theory contends that there is a small, highly innervated layer of fat which is affected in ITBFS and is the root of associated pain and reason for injury.
Whilst there has been no definitive answer as to the cause of this injury we do know that it hurts, a lot! But, with onset often spontaneous and the severely debilitating symptoms, many people struggle to identify why this issue has arisen.
HOW DOES ITB FRICTION SYNDROME OCCUR?
The primary cause of ITBFS is the Band’s anatomical positional change during gait. How it occurs is that when the leg is extended, the ITB is positioned behind the lateral epicondyle and axis of the knee. When the knee is bent (flexion) the ITB slides over the epicondyle to lie in front of it.
As this rubbing occurs hundreds or even thousands of times a day, altered biomechanics or sudden increases in loading can cause inflammation and degeneration of the band which is the hallmark of ITBFS.
As an overuse injury, the most commonly reported causes of ITFS are high or drastically increased training loads. Whether greater duration or more frequent sessions, rapid increase of the kilometers covered is a hallmark and one of the most recognizable symptoms of ITBFS.

WHAT ARE THE CAUSES OF ITB?
A major internal cause of ITBFS can be muscular imbalances or dysfunction. Weakness of our upper thigh muscles (adductor group) and those tasked with pelvic stability and posture (core, hip and gluteal muscles) can cause biomechanical or movement abnormalities.
Continued or prolonged exercise with poor posture and control will tighten up muscles (TFL and gluteus maximus), subsequently increasing the tension placed through the ITB.
This increase will cause the pathology and friction which creates ITBFS.
Poor foot arch control, specifically excessive pronation or collapsed arches can also cause ITBFS. As with muscle imbalances, foot position and arch control will determine movement patterns, possibly altering muscle length, activation and strength. As the arch collapses the lower leg will rotate and change the shape of the knee, increasing risk of friction.
External factors can also contribute to the development of ITBFS. Often reported and identifiable issues will include unsuitable running shoes (worn out or non-supportive), excessive hill training (especially downhill) or even running laterally along a hill.
These factors change the biomechanics of our running and can negatively affect technique, thereby increasing risk of injury.
WHAT ARE THE SYMPTOMS?
The primary symptom of ITBFS is pain over the lateral aspect of the knee. Pain is generally most severe in the morning or post-exercise as the body begins to cool down. During activity pain will usually begin as an ache which increases in severity and sharpness.
Pain will occur during activities of weight-bearing knee flexion and extension (bending) such as running, walking or squatting and can become severe enough to cause a limp.
In more advanced cases there may be swelling and inflammation present along the outer aspects of the knee and patients may experience crepitus, a grinding or popping sound present through movement.
If left untreated ITBFS can progress to a stage where there the knee may collapse, giving out due to pain. Before this occurs contact your physiotherapist for advice and treat of this knee pain.
HOW CAN PHYSIOTHERAPY HELP ITB FRICTION SYNDROME?
It is incredibly important to report to a physio if you suspect ITBFS, as treatment will be necessary to ensure a swift and complete recovery.
The first part of physio treatment will be diagnosing the injury. Correct diagnosis involves more than just identifying the presence of ITBFS. To remedy the injury, it is important that there is a correct diagnosis of the cause to direct and construct a beneficial treatment plan.
Our highly-trained physiotherapists will be able to diagnose both ITBFS and its cause through a comprehensive assessment addressing injury and exercise history, muscle imbalances/weaknesses or biomechanical and technique issues.
Once ITBFS and its mechanism has been identified progressive treatment will include a range of:
- Manual Therapy (via massage and trigger points).
- Joint mobilisation and manipulation.
- Reduction of pain and inflammation.
- Deloading of the ITB.
- Exercises to strengthen and mobilise the knee, hip and surrounding musculature.
- Education on causes and prevention.
- Bracing and taping.
- Improvement of biomechanics via remedying proprioception, balance and running technique.
- Ice/heat treatment.
- Dry-needling for muscle or fascia release.
- Gradual return to activity program.
ITBFS is usually treated conservatively with the methods above, however in the rare occasion that the injury requires further treatment via surgical release Pivotal Motion can refer you to the appropriate medical professionals to help aid in your complete recovery.
HOW TO AVOID ITB FRICTION SYNDROME?
Prevention of ITBFS is quite simple and mainly requires gradual increases in training load and the use of correct footwear or technique.
The main cause and sign of ITBFS that we experience in the clinic is a recent, large increase in training load. Generally involving running load, ITBFS can be avoided by gradual, progressive overloading as fitness and strength levels improve. By understanding your boundaries and not overloading too fast you can still get significant fitness or performance gains whilst staying healthy.
Making sure that you wear supportive footwear and orthotics (if required) when running is also important to avoid ITBFS. Excessive pronation through the feet will change the force loading through our knees and therefore can place extra strain through the knees which causes the painful friction.
Strong gluteals and hip muscles can also help to minimize risk of injury with ITBFS. As these muscles largely control the position and movement of the leg, strength will help maintain good technique and correct alignment throughout movement. For some great glute med exercises check out our blog on how glute med can trigger lower back pain here.
A solid and strong core will also assist in maintaining good posture throughout running and can help immensely with day-too-day function as well. Dry-needling such as planks and the pallof press will assist in strengthening your core and minimising risk of injury with activity.

If you are suffering pain after exercise, come see our friendly team at Pivotal Motion.
Book an appointment online or call us today on 07 3352 5116.

